Your feelings related to your blighted ovum miscarriage are valid, mama. If you’ve experienced this kind of miscarriage, you likely had all the symptoms of pregnancy and then suffered a shocking loss.
It’s okay to feel lost and alone, but please know that we are here to support you through your miscarriage journey. The following article is more of a science-based look at blighted ovum symptoms. If your heart needs more of a narrative story and you’d like to read more about my experience with a blighted ovum (my first pregnancy and miscarriage), you can find the full story here.
This site contains affiliate links, meaning that we earn a small commission for purchases made through our site. We only recommend products we personally use, love, or have thoroughly vetted.
- What You Need to Know
- Blighted Ovum Symptoms and Miscarriage: What to Expect
- Signs of Blighted Ovum
- Questions to Ask When You Have a Suspected Blighted Ovum
- Blighted Ovum Pregnancy Treatment Options
- Blighted Ovum Signs: More Questions to Ask the Doctor
- Your Blighted Ovum Pregnancy
- Blighted Ovum Pregnancy FAQs
What You Need to Know
- A blighted ovum (also known as an anembryonic pregnancy) occurs when a fertilized egg implants in the uterus, but the fertilized egg doesn’t develop into an embryo. A blighted ovum is the single leading cause of miscarriage.
- The hardest part of this kind of miscarriage is that pregnancy is that symptoms occur just like they would with a viable pregnancy. You’ll have a positive pregnancy test, and you may have morning sickness, achy breasts, food aversions, and other typical early pregnancy symptoms.
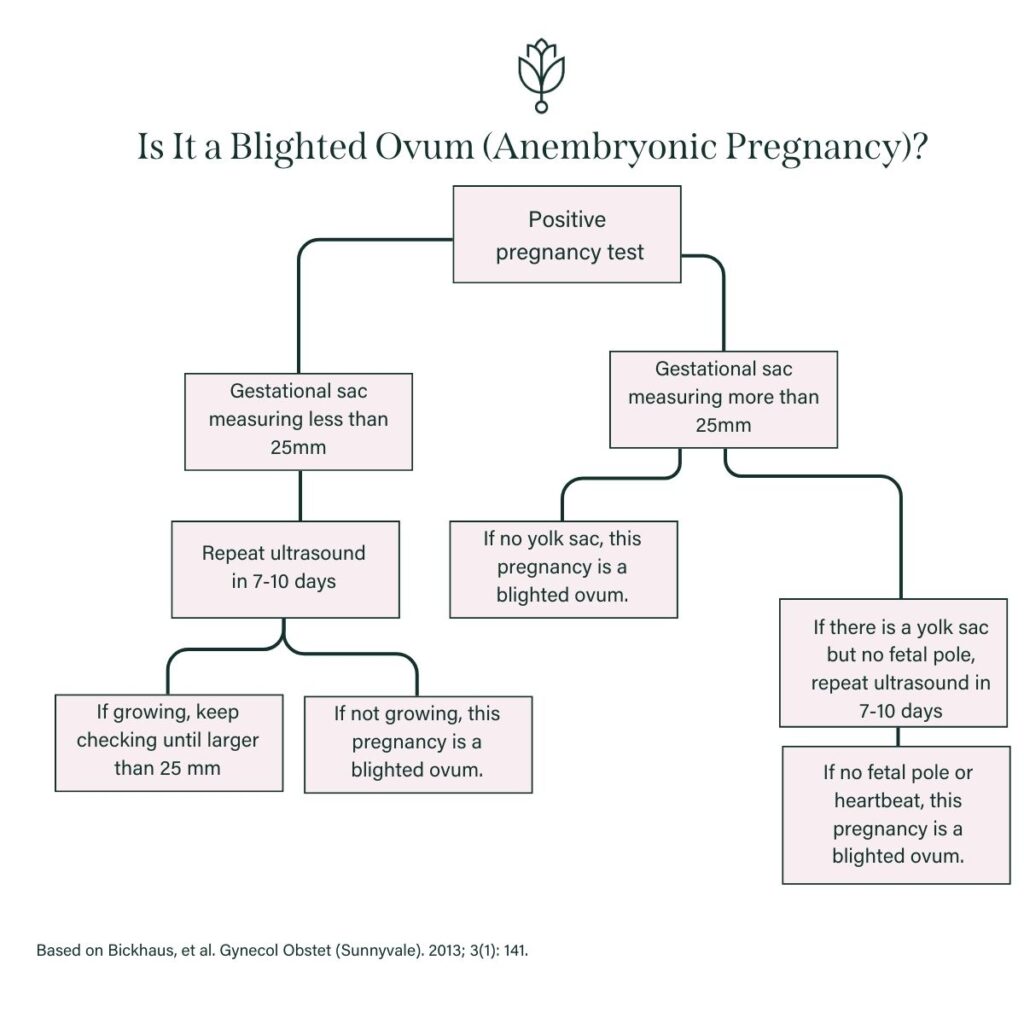
- The first blighted ovum sign is usually found by ultrasound around 7-8 weeks. Your doctor will notify you that they see a gestational sac, but no yolk sac, fetal pole, or heartbeat.
- If you know you have been tracking ovulation, you can confirm a blighted ovum by asking what your gestational sac measures. If your gestational sac is measuring greater than 25 mm but there is no fetal pole, your healthcare provider can confirm a blighted ovum, as well. You can also wait a week for a follow-up ultrasound to confirm that the pregnancy is not growing, but that’s a difficult wait, friend. I’ve been there.
- I’m so sorry, but if your doctor confirms a blighted ovum, this pregnancy is nonviable. Your treatment options are to take misoprostol to induce miscarriage, have a dilation and curettage (D&C), or wait to miscarry naturally.
Why trust us?
This article is a collaboration between Katy Huie Harrison, PhD, a seasoned fertility and women’s health advocate and blighted ovum miscarriage mama, and Samantha Radford, PhD, an expert in Chemistry and Public Health and our Resident Health Scientist. Edited by Sarah Creel, PhD
Blighted Ovum Symptoms and Miscarriage: What to Expect
One of the worst parts of a blighted ovum (BO) miscarriage is that it can feel just like any other pregnancy. Your human chorionic gonadotropin (hCG, aka “the pregnancy hormone”) levels will rise like normal. This is difficult because hCG triggers a positive pregnancy test and early pregnancy symptoms.
You may have:
- Morning sickness
- Cravings or food aversions
- Heartburn
- Bloating
- Sensitivity to taste and smell
- Fatigue
- Sore breasts
I’m so sorry, mama, but you can basically feel all the “normal” pregnancy symptoms, most likely without any early miscarriage symptoms.
In short: the problem with this is that you feel pregnant, but the pregnancy stops growing before an embryo develops. By the time your period is late, your chance of a healthy baby is already gone, but your body likely shows no signs of anything being amiss.
For this reason, it’s one of the most frustrating and heartbreaking types of miscarriage because it can take a long time to learn that your pregnancy isn’t viable.
Signs of Blighted Ovum
If you have a blighted ovum (aka anembryonic pregnancy), your ultrasound will show:
- No heartbeat
- No fetal pole
- (Possibly) no yolk sac
Questions to Ask When You Have a Suspected Blighted Ovum
When I first saw a blighted ovum ultrasound, I honestly had no idea what I was looking at. My doctor wasn’t in the office that day, and I should have had another physician answer my questions.
I didn’t know this at the time, so it doesn’t serve me to beat myself up for it now. This is why I’m sharing this information with you! If you go in for an ultrasound and you suspect a blighted ovum (no heartbeat or fetal pole), please ask a doctor to sit down with you and answer your questions.
You do not have to leave their office only to wait for a follow up ultrasound in a week to confirm miscarriage. You can ask questions now! We recommend asking the following:
1. Can You Find a Heartbeat or Fetal Pole?
Not being able to find a heartbeat or fetal pole is often the first sign that you may have a blighted ovum.
2. What Is My Gestational Sac Measuring?
If your gestational sac is measuring 25 mm or larger (around 7.9 weeks) but still has no fetal pole or yolk sac, this is a strong indication that your pregnancy isn’t viable.
Note: this is the guideline to diagnose an anembryonic pregnancy defined by the American College of Obstetricians and Gynecologists.
3. Is There a Yolk Sac?
If there is a yolk sac, there is still a possibility of a viable pregnancy. A repeat ultrasound would need to be scheduled 7-10 days later to see whether a fetal pole could be detected at that time.
4. How Long Should I Wait to Confirm My Blighted Ovum?
Generally, you’ll be told to come back 7-10 days after the initial ultrasound to confirm a blighted ovum.
Blighted Ovum Pregnancy Treatment Options
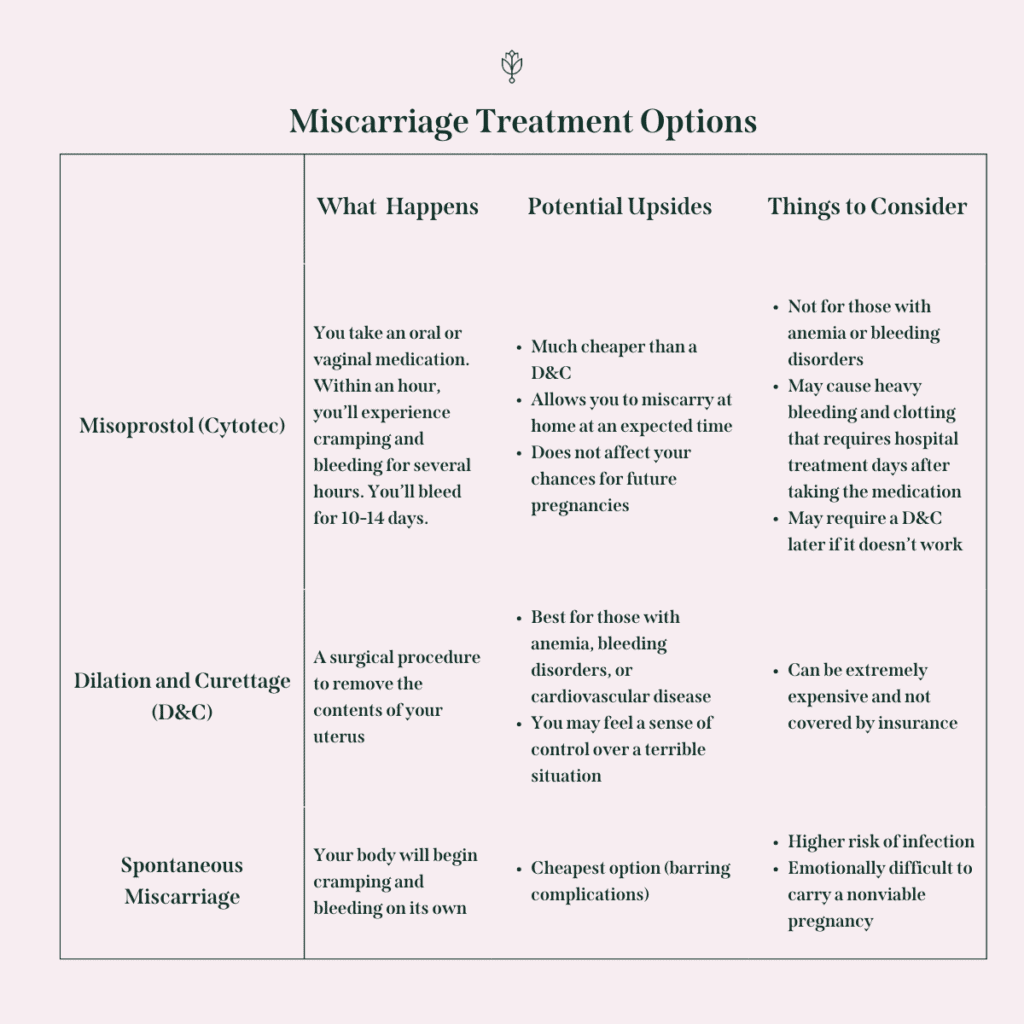
Once your care team has confirmed that you do, in fact, have a blighted ovum pregnancy, there are three primary blighted ovum treatment options your doctor should go over with you. Those options include:
- Take Cytotec (also called misoprostol), which is a drug that induces miscarriage when your body isn’t recognizing your loss (called a missed miscarriage). This is the most affordable medically-managed way to treat a missed miscarriage, but talk to your doctor ahead of time about risk factors and when to go to the emergency room if a problem occurs. Studies show that Cytotec alone is effective 78% of the time, with the remaining 22% of cases requiring surgical intervention, usually a D&C. Mifepristone can often be used with Cytotec to improve the rates of effectiveness, but it’s now illegal in states with a total abortion ban. If you choose to take Cytotec, we encourage you to have a support person at home with you in case you need extra care. Many people have scary experiences, like Arden, founder of The Miscarriage Doula, who wrote about her misoprostol miscarriage experiences for us. While less than 1% of people actually require blood transfusions or hospital admission due to the use of Cytotec, many end up in the emergency room either because their blood loss makes them fear they’re hemorrhaging or because the pain is too intense to be managed at home.
- Have a dilation and curettage (D&C), a surgical procedure where the doctor surgically removes the “contents of pregnancy” (don’t even get my started on that phrase; it’s so so terrible) from your uterus.
- Wait to miscarry naturally, but keep in mind that this process needs to be carefully monitored by your healthcare team to help prevent infection. Your hCG levels will need to be monitored to make sure they are going down.
Making a Decision about Treatment & Risks to Consider
Because of the surety of my blighted ovum miscarriage, my doctor discouraged waiting because of the physical and emotional toll such a decision would take on me.
Carrying a nonviable pregnancy can lead to infection and even sepsis, and knowing you’re carrying a nonviable pregnancy is extremely emotionally difficult.
Despite my doctor’s urging, I initially wanted to wait to miscarry naturally…until I spent that night on a towel on the floor, hovered around a toilet, and fully realized it was all for nothing. This pregnancy that was making me feel so miserable would never become a baby in my arms.
I had read far too many horror stories about Cytotec, stories like Arden’s misoprostol experience, and I knew I couldn’t handle the uncertainty of taking that medicine.
So, I opted for a D&C because it felt like the most controlled option to me.
Preparing for a D&C to end the physical saga of my blighted ovum story. The emotional and hormonal toll would continue.
I should mention that my D&C was freakishly expensive, but that many other miscarriage management options can be, as well. You can read more about that in an article I wrote on the financial and emotional cost of miscarriage for Romper.
Blighted Ovum Signs: More Questions to Ask the Doctor
If a blighted ovum is confirmed, here are other questions I would ask my doctor, if I were doing it all over again:
- Is there any chance of viability? Should we do another ultrasound in a week? (You never want to risk intervening in a pregnancy if you aren’t fully convinced it’s nonviable, even if your doctor is sure. It’s not fair to ever have to question your decision.)
- If you (the doctor) had to choose an intervention right now, what would you choose and why?
- How many of your patients who choose to wait to miscarry naturally or who take Cytotec still end up needing a D&C?
- How many of those patients end up in the ER during their physical loss?
- Do I have any physical restrictions right now?
- What are the restrictions on my daily life if I choose a D&C? For example, when can I exercise again, when can I take a bath, etc? What about if I choose a medically managed miscarriage (Cytotec)?
- What is the financial cost of a D&C? An ER visit if it’s necessary during miscarriage? (You may have to call your insurance company to answer these questions, U.S. mamas, but some hospitals and clinics have set pricing)
- If you choose a D&C, should we do genetic testing?
- Do you have the contact information for a good therapist who can support me through this time?
Your Blighted Ovum Pregnancy
I know that science-y information can be helpful for a lot of people while going through something medically traumatic–this is certainly the case for me! Medical information helps me feel prepared and in control. I hope this article makes you feel the same way, friend.
Don’t forget that a blighted ovum IS a pregnancy, and the loss you are feeling (if you experience it this way), is incredibly real. If you are struggling, reach out to your therapist, healthcare team, and people you love.
Blighted Ovum Pregnancy FAQs
Blighted ovums miscarry at different stages. Some occur as spontaneous losses very early. Others are not discovered until a first ultrasound, which can occur as late as 12-14 weeks gestation. They most commonly expel naturally between 7 and 12 weeks.
hG levels may be low with a blighted ovum miscarriage, but they can also continue to rise normally. hCG alone cannot determine whether a pregnancy is a blighted ovum. You will need a medical professional to determine blighted ovum via an ultrasound.
A blighted ovum may miscarry spontaneously, with bleeding and cramping like many other miscarriages. However, a BO can also be asymptomatic and feel like a normal pregnancy, requiring medical intervention after an ultrasound proves nonviability.
YES! When a blighted ovum occurs, a sperm and egg still come together, but a problem occurs as it develops into an embryo. A gestational sac implants into the uterine wall, and women produce pregnancy hormones and grow a sac. Early pregnancy with a BO feels just like traditional early pregnancy.
Blighted ovum miscarriages are relatively common, unfortunately. Up to 1 in 4 pregnancies is believed to end in miscarriage, and up to 50% of early pregnancy loss results from blighted ovum.
The reasons for a blighted ovum are unknown, but it’s suspected that most are caused by chromosomal abnormalities in what would normally grow to be the embryo. If you have a D&C, you can ask your doctor to test the gestational sac to determine if this was the cause.
There are instances of misdiagnosed blighted ovums, but they are very rare. This is why knowing how far along your sac is measuring is helpful. Blighted ovums are usually diagnosed by ultrasound, and it’s common to wait 1-2 weeks between ultrasounds. If there is any question in yours or your doctor’s mind about the viability of your pregnancy, then by all means, wait! Have a follow-up ultrasound. Feel certain. You never want to intervene in a wanted pregnancy only to wonder if your doctor was wrong. Be realistic. If you’re supposed to be 10 weeks pregnant and your gestational sac suggests that you are, but there was no heartbeat, I wouldn’t get my hopes up for the next ultrasound.









