
Aisha Stith is writing this article for her rockstar son, Chase, one of the most magnificent beings. And for everyone who has endured the trauma of delivering a child early. You see, Chase was born very early, at 30 weeks and 1 day. Aisha experienced both pregnancy and labor complications that reminded her of the benefits of patient empowerment, especially among African American women. Patient empowerment is something we must foster among US mothers. After all, the United States has the highest maternal mortality rates of any “developed country” in the world, and the statistics are even worse among African American women.
This site contains affiliate links, meaning that we earn a small commission for purchases made through our site. We only recommend products we personally use, love, or have thoroughly vetted.
Aisha’s Story: Pregnancy and Labor Complications that Required Patient Empowerment
I remember being wheeled through Northside Hospital, not quite in my third trimester. I was headed to an appointment with my perinatologist, a specialist that most pregnant women don’t even know about.
Perinatologists (also called maternal-fetal specialists) diagnose and treat complex maternal-fetal conditions.
It was at least my third visit.
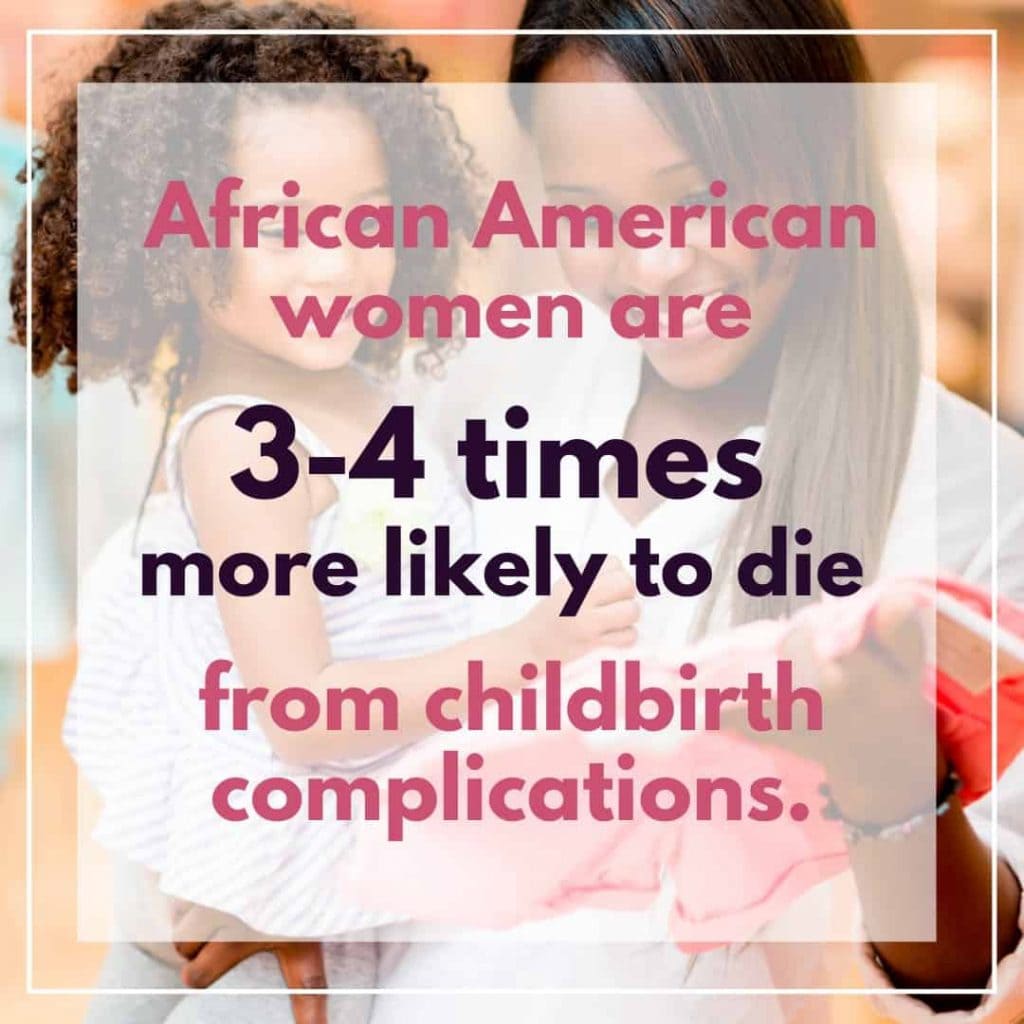
I turned around to the nurse and said, “This is so scary. Do you know about the statistics regarding black women in this country dying during pregnancy?” She was aware.
The nurse and I were all too familiar fact that African American women are 3 to 4 times more likely to die due to childbirth related complications than their white counterparts.
My husband quickly responded, “Don’t say that! Why would you say that?”
I never thought I was going to die. But I also never thought about the feeling of utter emptiness that this process would give me at my lowest moments. It was otherworldly.
There were warning signs about my health that appeared early on that I simply did not listen to–that my doctors did not listen to.
The message from this experience that I want to pass along to other women, especially women of color, is listen to those signs:
- Do what your body is telling you and, if necessary, be still.
- Take control of your actions and be mindful of a system that is struggling to meet the needs of your community.
- Advocate for your care if you need to. Be an empowered patient. It could be lifesaving.
Disparities in African American Maternal Care
The exposé featured an article on Shalon Irving, an epidemiologist at the Centers for Disease Control, who died of complications from high blood pressure only three weeks after giving birth.
National Public Radio’s (NPR) exposé of maternal mortality in the United States (2017), “Lost Mothers: Maternal Mortality in the U.S.,” blew the lid off disparities between maternal care for white and black women.
The statistics the article reveals are taken from the very pinnacle of health expertise: the CDC. The same place where Shalon Irving, PhD worked as an epidemiologist.
These statistics are daunting, mystifying and downright terrifying:
“Black mothers in the U.S. die at three to four times the rate of white mothers, one of the widest of all racial disparities in women’s health. Put another way, a black woman is 22 percent more likely to die from heart disease than a white woman, 71 percent more likely to perish from cervical cancer, but 243 percent more likely to die from pregnancy- or childbirth-related causes.”
If it’s not clear from Shalon Irving’s story–the story of a woman with a PhD in SCIENCE–it’s clear from these hard statistics.
Me, a mother of two healthy children and one on the way, had every right to be concerned about being an African American woman in the care of a high-risk pregnancy specialist.
I was lucky in that I knew I was in a good hospital, but things can go wrong anywhere. I wish I had better understood the need for patient empowerment, should it be necessary.
Lack of Patient Empowerment and Pregnancy Complications
Getting pregnant with my third child, Chase, was like a dream.
I was 34, and I had just recovered from a minor surgery to remove my fibroids. Thankfully, the surgery had gone seamlessly.
I really wanted to have my third baby at the age of 35, but as the adage goes, be careful what you wish for.
Note: The risk of pregnancy complications was greater because of the fibroids. Fibroids and preeclampsia are 3 times more likely to occur in black women than in white women, according to ProPublica. In fact, 80% of African American women have fibroids, and no one knows why.
Appearance vs. Reality
From what the doctor could see, I was “healthy.”
I was happily married. I had 2 amazing children and 2 prior easy pregnancies with “no prior complications.”
Seemingly a perfect time and place to have a baby, right?
What I knew about my body and my readiness to have another baby was different.
I Was Not an Empowered Patient
I knew that I was overweight and that I had gained too much weight during previous pregnancies, despite actively trying not to. I also knew I had not lost a significant amount of weight after my previous pregnancies, despite trying.
During my previous pregnancies, I had remained active, sometimes going to the gym daily. I ate a sensible diet for a pregnant person, and I told myself, “After my third baby I will make sure the weight never comes back.”
Many women deal with postpartum body image challenges, but this was different. I tried, but I just couldn’t figure out why I couldn’t lose the weight.
I sought medical help and spent thousands of dollars trying to solve this problem. But I have felt over the years that medical professionals have not taken my health seriously.
This is where patient empowerment becomes so important, and I wish I better understood the need to advocate for myself.
So What Is Patient Empowerment?
The World Health Organization defines patient empowerment as “a process in which patients understand their role, are given the knowledge and skills by their health-care provider to perform a task in an environment that recognizes community and cultural differences and encourages patient participation.”
There are four components that are fundamental to the process of patient empowerment:
- Understanding by the patient of his/her role;
- Acquisition by patients of sufficient knowledge to be able to engage with their healthcare provider;
- Patient skills; and
- The presence of a facilitating environment.
Clearly, I was not missing number two. I knew how to engage with my healthcare provider. I am an educated woman. But what I was missing–that this definition doesn’t acknowledge–is that while I was relaying many symptoms that can be precursors of serious pregnancy complications, my doctor did not take me or my concerns seriously.
So I added to this definition: patient empowerment also involves a certain amount of tenacity for all mothers.
Unfortunately, our healthcare system is set up in a way that we have to fight to be heard and understood. This especially applies to African American mothers who have a much higher maternal death rate.
Why is Patient Empowerment Important?
Patient empowerment is important because it means that the patient recognizes her own role in pregnancy and childbirth.
Thankfully, we no longer live in an age where women are required to be passive during the experience of carrying and birthing children. But we do live in a time where women still aren’t always heard regarding our own bodies.
Patient empowerment is important because it lets your doctor know that you refuse to have your concerns taken lightly. You demand to be heard.
As such, you should always tell your doctors when you know there’s a problem, or even when your medical team suspects one.
If they don’t take your concerns seriously, push for them to investigate further. If they refuse, find a care provider who will investigate further.
Note: And this is an important note. By discussing the need for patient empowerment, we are in no way intending to cast blame on patients whose needs haven’t been taken seriously. You did nothing wrong. You very probably pushed and still weren’t taken seriously. It should not be your job to be your own advocate. Because it seems like it has become your job, however, we do want to help provide the tools to allow you to advocate for yourself.
Advocating for Myself During Pregnancy: What I Wish I Had Known
I did not advocate for myself in the time leading up to my third pregnancy, and I wish I had. I’m here to help you learn how.
I am knowledgeable and, in many ways, privileged. Yet I kept getting the “just don’t eat rice and potatoes,” speech from my doctors in regards to my weight.
Needless to say this was beyond annoying and completely unhelpful.
In retrospect, do feel I should have advocated for my health before pregnancy.
I recently read that Teddi Mellancamp, of Real Housewives and Vanderpump Rules fame, will celebrate her third pregnancy for the first time as a “fit and healthy” woman. I am so proud of her, and anyone who accomplishes this feat.
But even while I feel like I should have advocated more for my health and the questions I had regarding my inability to lose weight despite diet and exercise, guess what?
My healthcare team should have also questioned this issue.
It should not be my job to be my own advocate, but one of the benefits of patient empowerment is that you can be if needed.
Pregnancy Complications with Chase
By the beginning of my seventh month of pregnancy, I was exhausted in a way that I can not describe. Yet I didn’t stop.
My doctor told me that my blood pressure was dangerously high and that I would need to go on bedrest. I was terrified.
I had my entire pregnancy planned, down to my leave from work, and this completely threw everything off track. Or so I thought.
I could not wrap my head around bedrest. I continued working a stressful job, albeit from home, but I left every day to get my kids. I also entertained them, cooked, and even hosted family members for visits.
As things took a turn for the worse, people would come over and do that thing. You know, that thing where they would lean over me, squint and say “Aisha you don’t look so good.”
My response was always, “I am seven months pregnant, what do you expect a swimsuit model?”
Despite my humor, I was scared.
And given the statistics about black women’s maternal mortality rate, I had every right to be.
I knew my blood pressure was high. Had I researched fibroids before pregnancy, I would’ve known I was at an increased risk for preeclampsia.
Again, this is something my doctors should have told me, but sometimes doing your own research is part of being your own advocate.
Edema, Preeclampsia, Bedrest, and Delivery
One night, my entire body felt like a water balloon. My face, hands, and feet were swollen, and I thought it had to be edema, otherwise known as excess swelling.
I checked into the hospital for the second stay of my pregnancy with Chase. I remained there until his birth.
I had edema of course, but worse, my urine protein showed I had developed preeclampsia.
Honestly, I had only heard this term once. Remember, my previous two pregnancies were healthy.
I’d only heard about it when Kim Kardashian spoke about not carrying more children on her own because of the condition. In other words, what I knew was the preeclampsia was dangerous and scary, and doctors should’ve told me my risk factors.
Why Didn’t I Slow Down, Even While on Bedrest?
Part of the reason I didn’t stop and listen to my body was that I felt guilty about being sick. Mom guilt is very real, and my kids were used to a fun, engaged, active mommy. I felt serious parenting guilt about the fact that I had become the opposite of what they had known before my third pregnancy with Chase.
Also, I had adjusted to being overweight, so it was harder to recognize that I was unhealthy. My doctors never helped me understand that there were connections to preeclampsia and being overweight.
I had multiple risk factors for preeclampsia, but no one warned me until I developed it.
Being on hospital bedrest wasn’t worth any activity I attempted to complete. I kept wondering, “Why didn’t I slow down?”
I can’t help but wonder if I would’ve taken bedrest more seriously had anyone bothered to explain how serious my complications could be.
Labor
After a week in the hospital, with no safe way to lower my blood pressure, the perinatologist said, “We are going to need to deliver this baby.” I was 30 weeks and 1 day.
I knew it was time to deliver, and I just prayed that we would all make it through and be able to thrive on the other side.
The delivery seemed normal, and the staff at Northside did a remarkable job of treating me as if I were going to be okay.
There were, of course, three times the number of nurses than a normal birthing room, but the room felt calm and supportive.
This is one way in which my care team really supported me. I was lucky to be at such a good hospital, and that I didn’t need to worry about patient empowerment or being my own advocate during birth (even when this wasn’t the case leading up to Chase’s birth).
My husband morphed into a superhero. He was everywhere for me and my children.
Chase’s Birth
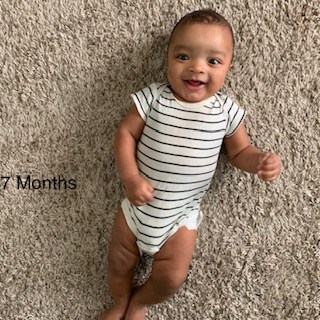
My son came into the world extremely healthy for a baby born at his gestation. One nurse even let me hold my tiny 3.4lb son before he was rushed to the NICU.

I hope she knows that those three seconds gave me the strength to get through a very otherworldly experience over the next five weeks.
I am now on my journey to living my best life. My son is seven months old and on par with his peers in nearly every category. We are so blessed.
I am on a mission to get healthy and to empower and inform women on their pregnancy journey. I am motivated and excited to live a truly healthy life and encourage others along the way.
Advocating for Black Mothers to be Empowered Patients
But this is not the story of every black mother who experiences such complications. I mentioned Shalon Irving, PhD, earlier in this article. She was another seemingly privileged black mother who also gave birth–and died from pregnancy complications–in Atlanta.
And here’s another scary detail. According to Shalon’s mother, Wanda, Dr. Shalon Irving was an empowered patient.
She knew she was at greater risk for a complicated pregnancy due to a blood clotting disorder. She took daily medicine (editorial note: likely by giving herself a daily shot in the stomach, although we have not confirmed this detail) to control this risk factor.
She had a birth plan, and she visited her clinic multiple times after giving birth because she knew her spikes in blood pressure, pain, headaches, and swelling, were not normal.
(Another editorial note: these are all symptoms of preeclampsia or eclampsia, the extremely dangerous condition that can follow preeclampsia. Other symptoms of preeclampsia include vision changes and pain in the upper right quadrant of your stomach. Eclampsia symptoms are similar, but more severe, including nausea/vomiting, change in mental status, seizures, and more. Many symptoms overlap. If you experience these symptoms postpartum, go to the ER.)
Even though Dr. Irving was clearly an empowered patient, she died of complications from high blood pressure (a symptom of eclampsia) only three weeks after her daughter was born.
Although these tips are good for everyone, they’re especially important for African American mothers due to their greatly increased maternal mortality risk.
3 Tips for Practicing Patient Empowerment as an African American Mother
- Have a postpartum plan. Everyone talks about birth plans, but Irving’s mother wonders whether her daughter might have lived if she’d had a postpartum plan. We all know that postpartum recovery is hard. But being aware of the difference between normal postpartum discomfort and major postpartum complications–and what you’ll do if you experience major complications–could be a game changer. Find extra resources to learn about postpartum complications here.
- Teach your support network about risk factors. During the second trimester of your pregnancy, learn your risk factors and talk to your support network about them. Write them down. If things go wrong, you may not be able to be your own advocate, but those around you still can.
- Find at least 1 support person who is willing to be fiery. It is not fair that you need to advocate for yourself in medical situations, but whether fair or not, the possibility is a reality. To fully practice patient empowerment, know that you have a person who supports you who (1) knows the warning signs and (2) will push until doctors take your concerns seriously.
Hopefully, none of this preparation will be necessary. Again, it shouldn’t be your job to advocate for yourself in medical situations. But if you have to, you’ll be so thankful you were prepared!
Tell us about your experience with patient empowerment.









3 thoughts on “The Benefits of Patient Empowerment for African American Mothers”