When Husband and I finally decided to try to conceive (TTC), I thought it would be easy. I never imagined I’d find myself navigating the worlds of infertility and recurrent miscarriage. I don’t think any of us envision ourselves in those places, and yet, we so often end up there.
It’s the sort of invincible complex we all have–those bad things will happen, but they won’t happen to me. Until they do.
Until I’d spent a year-and-a-half trying to get pregnant, only to have it happen and immediately find myself in the gut-wrenching throws of recurrent miscarriage.
I’ve mentioned our journey with recurrent miscarriage, also called recurrent pregnancy loss (RPL), many times.
I first mention it in “My Arduous Journey to Becoming a Mother,” and get a bit more in depth in my controversial article “#CallitPregnancyLoss: How Our Words Have Devastating Power.” In this article, I argue against the use of the word miscarriage. But I continue to use that word anyway because I know it’s what most people search for, and I want you to find these resources when you need them.
In this article, I finally tell our story. Buckle up–it’s a hell of a ride.
This is a long post, so I’m providing a quick Table of Contents to guide you through it.
This site contains affiliate links, meaning that we earn a small commission for purchases made through our site. We only recommend products we personally use, love, or have thoroughly vetted.
- Trying to Conceive
- The Beginning of Recurrent Miscarriage: A Blighted Ovum
- Trying to Conceive After Miscarriage
- A Chemical Pregnancy Welcomed Me to Recurrent Miscarriage
- Next Steps: Recurrent Miscarriage Testing
- Tests and Confusion
- An Ectopic Pregnancy
- Recurrent Miscarriage Testing
- Recurrent Miscarriage Support Resources
Trying to Conceive
I believed the myth that my pregnancy experience would look just like my mother’s. She got pregnant on her honeymoon, had easy pregnancies, and her labors were a breeze (as far as labor goes).
So Husband and I went into this process with serious rose-colored glasses. Like, I cannot emphasize enough just how rose-colored.

Planning A Pregnancy
Let me begin by talking about the absolute absurdity of this notion of “planning” a pregnancy. When Husband and I first began trying to conceive, we were sadly naive.
Here’s the deal.
I was in graduate school and was writing my doctoral dissertation. For those of you lucky enough not to know the grad school lingo, that basically means I was writing a big ole book full of research and words most people don’t want to say or read.
It’s called Surrogate Power, the Agency of the Replacement Mother in Mid-Victorian Literature. What do you think? You don’t want to read it?
Yeah. Me neither, and I wrote the damned thing.
Anyway. As I was writing this beast, I thought (again naively) that it would be a good time to have a baby. But it needed to be a summer baby so I could fulfill my teaching obligations–as a grad student, I wasn’t entitled to maternity leave, and most graduate students are in the same boat.
We timed our efforts to ensure the baby would be born in May or June. But–GASP–we didn’t get pregnant! We were honestly surprised. Really?!
After just 2 months of trying, we were like, “WTF? We aren’t pregnant? What are we supposed to do now???”
Fear and Uncertainty
We decided to keep trying, though not as seriously at this point. I wasn’t tracking ovulation or any of that. But every month I hoped, assuming we’d figure out the lack of maternity leave later.
Nothing happened. Eventually, I almost forgot about it.
Except for one September, when I traveled to Santa Barbara to celebrate my friend Christina’s 30th birthday with a bunch of her girlfriends. By the time I got to California, I was almost 10 days late–with all negative pregnancy tests. I took one every day.
Christina is an OBGYN (at the time, she was in residency), so I confided my situation. Well, I confided part of it. At this point, no one knew we were trying to conceive, so I just told her I was late but getting negative pregnancy tests.
There were plans for lots of wine. Should I drink it?
She assured me that having an abnormal cycle once or twice a year is normal, and that at this point, a pregnancy test should be able to pick it up if I were pregnant.
“It’s possible,” she said, “because you could’ve had a cycle where you ovulated later than normal and it’s still too early to detect. But it’s likely it’s just an off cycle.”
I confided my greatest fear.
“I’m afraid I started to get pregnant but something went wrong, and that’s why I’m not getting a period or a positive pregnancy test. I’m terrified I’m walking around carrying a dead baby and just don’t know it.” (Note: I realize this language sounds insensitive, but it was my spiraling, terrified, confused thought process.)
The thing is, I had no idea what I was fortelling.
The Beginning of Recurrent Miscarriage: A Blighted Ovum
It took another year to get pregnant. At this point, we’d been trying for a year-and-a-half.
I was sitting on the couch with Husband, making a list of questions to ask my gynecologist at my annual checkup the next day. Because that’s how timing works.
Husband was researching fertility testing, and I was making my list.
Suddenly, I felt a sharp pain in my left breast. This is when it hit me.
I had been nauseous all weekend and abnormally craving chicken sausage from a nearby restaurant. But I’d become so accustomed to negative pregnancy tests that it literally never occurred to me I could be pregnant. Hell, I’d had a bloody mary at brunch that very morning.
I said nothing to Husband about my new suspicion, but I ran to the bathroom, took a test, and saw 2 dark pink lines immediately. No waiting 3 minutes. Or even 2 or 1. There they were, bright, unmistakable.
I was pregnant.
The First Ultrasound
I was pregnant…until I wasn’t. My gynecologist confirmed my results the next day. She started monitoring my HCG (“the pregnancy hormone”) levels. They were rising appropriately.
Once I reached 6 weeks with HCG levels over 3,000, it was time for an ultrasound. According to my doctor, that’s when you should be able to see a heartbeat. Or at least the fetal pole that is sort of the pre-heartbeat.
My doctor was out that day, but for a routine ultrasound, we didn’t worry about her absence.
I sat in the waiting room eyeing the other couple obviously there for their first ultrasound. “We’ll have our babies at the same time,” I thought. “I should befriend her.”
Thank God I didn’t.
Eventually, we were ushered into the ultrasound room. I was instructed to empty my bladder and undress from the waist down.
When I sat down and put my legs in stirrups, Husband was MORTIFIED.
“What are they going to do to you?” he asked, stunned. He suddenly realized how thankful he was to be male.
The ultrasound technician searched and searched, then stood up and said, “I’ll be right back.”
Something Was Wrong
As she left the room, I started shaking and crying. “Something is wrong,” I told Husband.
“Why do you think that?” he asked. “She didn’t say anything was wrong.”
“She’s not allowed to,” I told him. “She went to get a doctor to tell me.”
“But this is not how these things go. When you have an ultrasound, they find the heartbeat, turn up the volume so you can hear it, and turn the screen to you to show it to you. She never let me see the screen. She never turned up the volume. SOMETHING IS WRONG!”
Husband comforted me as best as he could, remaining only slightly more optimistic. When the ultrasound technician returned, she said that she’d been searching for a doctor but they couldn’t find one. So, she explained what she could.
“I don’t see anything right now,” she said. “Your gestational sac is growing, but I don’t see anything inside of it. You’re probably just earlier than you think.”
“How worried should I be?”
“I’m not supposed to answer that, she said, but I’d say it’s 50/50 at this point. Make an appointment on your way out to come back in a week, but make sure your doctor is here the day you come. We’ll be able to tell for sure then.”
Seeing how scared I was, she tried to reassure me. “You’re probably just earlier than you think.” Those are the words we left with.
Questions I Wish I Had Known to Ask
- “When you say you don’t see anything, what does that mean?”
- “You see a gestational sac, but do you see a yolk sac? Do you see a fetal pole?”
- What is my gestational sac measuring?
Had I asked these questions, I would’ve learned that there was nothing inside the gestational sac, but it was measuring 7 ½ weeks. If I’d had that information, I’d have known this was not a viable pregnancy.
I wouldn’t have spent the next week hoping, praying, convincing myself that things were fine. I wouldn’t have been so devastated when we confirmed the truth.
Follow-Up Ultrasound
A week later, I returned. I saw the same technician, who to this day I can’t lay eyes on without my stomach churning. She completed the ultrasound routinely, then sent me to my doctor.
“I’m so sorry,” my doctor said.
“I’m also sorry I didn’t call after last week’s ultrasound. I was going to, but then [the ultrasound technician] told me she’d explained that you were very likely going to lose this pregnancy, and she said you seemed okay.”
This is when I began fuming. My blood began to boil. That is NOT what she told me! She gave me false hope. A lot of it.
I had spent the past week waiting for cramps and blood, and never experiencing any. So I’d convinced myself that everything was okay. But it wasn’t okay.
And the ultrasound tech knew it. She just didn’t tell me. F*ck her!!!!
This was the narrative in my head. To my doctor, I just nodded.
I was so angry, so devastated, so utterly broken, that I couldn’t make eye contact. I pulled out my phone and started texting people to tell them what was happening.
I had to assure my doctor I wasn’t videoing her. I just couldn’t look at her. I couldn’t handle any of it.
All I wanted was to be home on my couch.
The Aftermath of A Missed Miscarriage
When I made it to my couch, I crumbled. I couldn’t take another step. I felt like my life was ending.
I don’t mean that I wanted to end my life. I mean that I genuinely felt like my heart was beating so rapidly that it might explode. And like the darkness I saw was so all-encompassing that I had no idea how to walk through it back into light.
I sent Husband to get cookie dough and Annie’s cheddar bunnies, which became my primary diet during recurrent miscarriage. I turned on Gilmore Girls, snuggled with my dogs, and cried for days.
Friends sent flowers and food, and I’ll be eternally grateful for that. My friend Mary showed up at my house with a miscarriage care package.
I didn’t want her there. I was angry when I saw her at the door.
I had sent Husband back to work because I wanted to be alone. (I somehow never considered whether going back to work was what he needed in that moment. Honestly, it never occurred to me in the early moments to realize that he’d just lost the child he’d dreamed of, too. I’m sorry for that, Husband.)
But I opened the door to Mary. I’m so thankful I did. Support systems are key, y’all. We need people who know how to support someone after miscarriage.
She came with smutty magazines, gatorade to stay hydrated, sea bands to help with nausea, and Unisom to help me sleep.
“These are all pregnancy safe,” she explained. “I know that doesn’t matter, but I also know you won’t take anything that isn’t yet.”
Y’all. There is nothing better than having a support system of people who know you. Like, REALLY know you. This kind of care was essential, even though I didn’t think I wanted it.
A Decision: Surgery Or Medication
When I left the doctor, I’d wanted to wait to miscarry naturally. I didn’t entirely believe what was happening—shock and disbelief are early parts of grief, after all. By losing the pregnancy naturally, I would know it was really over.
My doctor considered this plan both emotionally and physically unhealthy. But she recognized my bodily autonomy, because she’s wonderful, so she came up with a compromise.
She’d give me 2 weeks, but I’d have to be monitored. If I started developing any sort of infection (which can happen at this point), or if things started to go downhill, we would intervene.
I agreed.
She sent me home with a prescription for Cytotec (to induce miscarriage) and pain meds, just in case I changed my mind. This put some of the power back into my hands, which I appreciated.
When Mary came over, I told her what I wanted and why. She didn’t judge, though she did offer insight based on all she knew about me and how my brain worked. After over an hour of discussion, I was nearing a very different decision–I wanted surgery to end the pregnancy (a D&C).
That night, I found myself on the cold bathroom floor, wearing my sea bands for nausea, hugging the toilet from “morning” sickness.
This is the cruelest trick of a “missed miscarriage,” where your body doesn’t recognize the loss. Your body acts completely pregnant.
“What the hell am I putting up with this for?” I asked myself.
The next morning, I scheduled a D&C.

I made this choice because it felt the most controlled. When everything else in my life seemed to be spinning out of control, I could control this one thing.
Decisions I Wish I’d Made Differently
- Deciding on the D&C sooner
- Having the gestational sac tested
After a D&C, you have the option of having testing done on the fetal tissue to look for chromosomal abnormalities. (Chromosomal abnormalities are the primary cause of miscarriage.) Since I had no fetal tissue, they still could’ve tested the gestational sac.
I didn’t want to do this for 2 reasons:
- It was my first loss, and it wasn’t *statistically* likely I’d have more
- I would learn the sex from those results, and my heart couldn’t take that
Here’s why I wish I’d done it.
We learned MUCH later, and after much heartbreak, that a problem with my uterus likely caused my losses. Had we tested the gestational sac and found no chromosomal abnormalities, it might have guided later recurrent miscarriage testing.
We might’ve moved to testing for anatomical abnormalities sooner.
Because of my later types of losses, I didn’t get another chance to test.
Trying to Conceive After Miscarriage
We waited one cycle and then began trying again. Trying to conceive looked VERY different now.
No more trying and hoping. That had taken a year-and-a-half. I had just felt like our dreams were finally in our grasp, only to have the life I dreamed of ripped away. I was not ready to wait another year-and-a-half for another chance.
I learned the best ways to track ovulation. I invested in a fertility monitor and we were pregnant within 2 months because I learned so much about my cycle. Obviously not everyone will have that level of success, but it’s telling how much I didn’t understand about my own body.
*Note: Trying to conceive after miscarriage is a total mindf***. Pregnancy after miscarriage is possibly worse. Check out this article on managing pregnancy anxiety after miscarriage.
A Chemical Pregnancy Welcomed Me to Recurrent Miscarriage
Thanks to the technology of fertility monitoring, we were able to get pregnant quickly. It was as if a switch had flipped once I’d been pregnant. I couldn’t get pregnant for a year-and-a-half. After I got pregnant once, I couldn’t stop.
After 2 months of trying, I was pregnant for the second time.
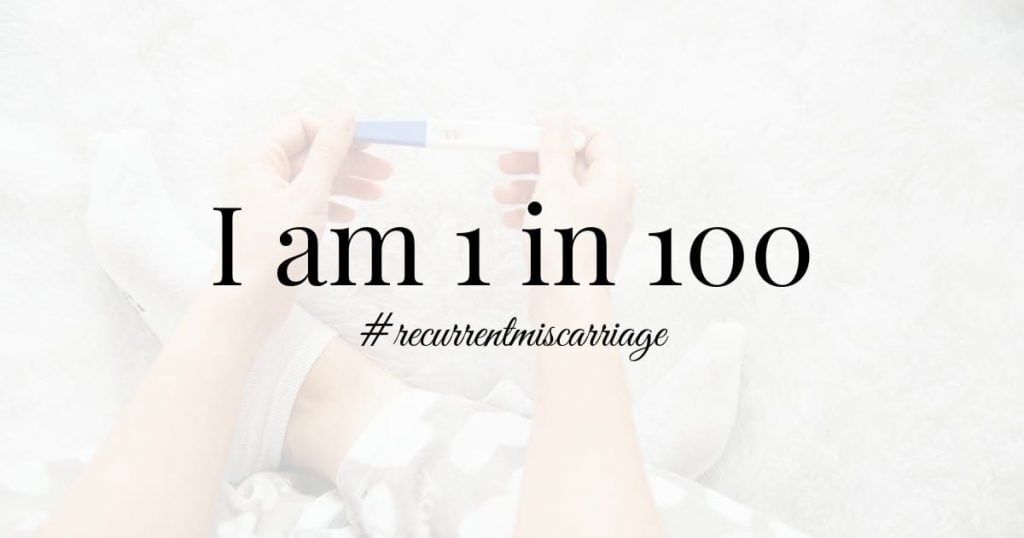
My hormone levels were again rising normally, and we had our first ultrasound on the calendar. The chances of losing another pregnancy was slim–back-to-back miscarriages are rare. They happen to less than 1% of women.
Husband and I had tickets to see The Book of Mormon at the Fox Theatre, and I was driving us down in afternoon traffic when I began cramping. “These cramps don’t feel right,” I said to Husband. “They really don’t feel right.”
I didn’t know what to expect when miscarrying because I’d previously had a D&C, but I knew these cramps were too intense to be normal.
Unable to do anything about it in traffic, we tried to think positively as we made our way to dinner. We’d been seated at dinner for 5 minutes when I couldn’t take it anymore.
“I’m going to the bathroom,” I said.
And so I did.
And there it was. Bright red blood.
I took a deep breath, tried to pull myself together, and walked back out to find Husband. “We need to leave,” I said. “I’m losing this one too.”
He looked at me with pain in his eyes, not sure what to do. Finally, he spoke.
“I don’t know what to say or do right now,” he admitted. “But I’ve already ordered our burgers, and burgers don’t take long, and we have to eat.” Long pause. “What do you think?”
“Order me a milkshake,” I said. “I’ll go try to contain this.”
So I stuffed my underwear with toilet paper to act like a sanitary pad, and Husband and I sat at a bar, eating our burgers and drinking a milkshake, having a miscarriage.
We didn’t say a word. We just ate and left.
Next Steps: Recurrent Miscarriage Testing
I called my doctor’s emergency line on the way home, and when she returned my call, I could hear the tears in her eyes.
It was Friday night. I should rest all weekend, use the pain medicine from after my D&C if I needed it. I went in Monday for a blood test, which confirmed the loss.
I only bled and cramped badly that night. Then it went away for a full week, until the next weekend when I spent 2 days finally, fully losing that pregnancy. That’s one thing I didn’t know to expect about miscarriage. It doesn’t necessarily happen all at once.
I was no longer 1 in 4. I was now 1 in 100.
I was lucky in that my doctor knew how rare that was.
Most doctors make you wait until you’ve had 3 miscarriages to begin testing, but mine wanted to start after 2. I was going to be able to begin a full recurrent miscarriage workup faster than most people.
Because just by happenstance (or, as I believe, fate), her husband was a fertility specialist, a Reproductive Endocrinologist to be exact. He would get me into his schedule as quickly as possible (which still isn’t quick when you’re going through it) to begin the recurrent miscarriage testing process.
All we had to do first was monitor my HCG (pregnancy hormone) levels until they were at 0. Then I could begin testing.
Conception and Miscarriage: Always Expect the Unexpected
It took a while to get there.
Those hormones just weren’t lowering fast enough, but they were decreasing. So, my doctor wasn’t worried we needed to intervene.
(Intervention would’ve meant either taking Cytotec or having another D&C–the first of which I wanted to avoid, and the second of which my doctor wanted to avoid).
*Note: When you hear people complain that doctors like you to believe a pregnancy isn’t viable so they can make money off of terminating it, please consider the reality. My pregnancies absolutely, with plenty of proof, were not viable, and my doctor always recommended the option that cost me the least and earned her the least. I didn’t always choose those options, but she always recommended them.
I was in my office one day with my office-mate and friend, Rebekah, when my doctor called.
Certain that she was calling to tell me my hormone levels were finally at 0 and that I was cleared to begin fertility testing, I answered in Rebekah’s presence.
“Can you sit down?” my doctor asked.
Huh?
“Have you had sex since your last loss?” she asked.
I began to stutter, confused. “Umm, once,” I muttered, “but only once, and we were careful. I mean, not like I’m on birth control, but we were careful.”
“Not careful enough,” she said, trying to be lighthearted. “You’re pregnant. I need you to come in for blood work. Now. If you’ll give me permission, I’ll consult with my husband to find out what tests I can safely run to see if there’s anything we can do to save this one.”
Tests and Confusion
I gave her permission, packed my things, and left for the doctor’s office in stunned disbelief. “A mixup at the lab,” Rebekah and I kept repeating, as I was sure another pregnancy meant another loss. “A mixup at the lab.”
(Note: If you want to learn how to support someone after a miscarriage, Rebekah is an amazing example. I tell how she helped me by validating my grief here.)
They drew 20+ vials of blood at the doctor’s office that day to run every test they could think of, including one to test my hormone levels.
We would get those test results back in 2 days, and in the meantime, I continued repeating my mantra.
“A mixup at the lab.”
I truly never allowed myself to believe I was pregnant or to become attached to this pregnancy. I knew it would end. I was certain of it.
So I just repeated this mantra all day, everyday.
“A mixup at the lab.”
An Ectopic Pregnancy
2 days later, I was again in my office with Rebekah when my phone rang. Rebekah was already well in on the madness, and had actually just told me she was pregnant herself. It was an interesting dynamic we were about to have to navigate.
So I answered the phone.
My doctor knew I wasn’t attached this time. She knew I didn’t want to believe it, so she was much more matter-of-fact in her tone, which worked for me.
“Well, we tried,” she said.
“Should I expect to start bleeding soon?” I asked.
“No,” she said. “I actually need you to go to the emergency room. I think this one is ectopic.”
Now, I’m sorry, but hold up just one damned minute here. ARE YOU EFFING KIDDING ME????? I’ve been going through all of this shit just to end up with a pregnancy in my fallopian tube???? This was unacceptable, universe. Simply unacceptable.
I raged internally, and a little to Rebekah, and then I went home so Husband could pick me up and take me to the ER.
I was taken back after about an hour of waiting, and an ultrasound confirmed that the pregnancy was indeed, ectopic.
Luckily, we’d found it so early that it hadn’t had time to cause problems. I was given a shot of methotrexate and sent on my way.
And weirdly, that was it.
I was very lucky it wasn’t more serious. To know more about how serious an ectopic pregnancy can be, read Beth’s ectopic pregnancy story.
Because methotrexate, and I know this sounds so weird and terrible, literally dissolves the pregnancy.
My pregnancy dissolved without so much as a cramp or a drop of blood. It was eerily like it had never happened, especially since I had never accepted that it was happening at all.
Recurrent Miscarriage Testing
And so, the recurrent miscarriage testing began. One thing people don’t tell you before you start trying to conceive is how much time you spend waiting.
Waiting to ovulate. Waiting to be able to take a pregnancy test. To take another one. For blood tests and ultrasounds. Or for the next month to pass so you can try again.
Once you start recurrent miscarriage testing, the waiting game is a whole new mess. There are a lot of women trying to get into fertility clinics, so they’re pretty full–just getting to see a specialist is a waiting game.
And when you’ve been playing this TTC/recurrent miscarriage game for years now, a few months to get into a specialist feels like forever.
When you finally get in, it’s for a consult. Then the doctor has to decide what tests to run. Then they have to schedule them. Often, you have to wait until the 14th day of your next cycle, or until during your period.
And your schedule has to align with the doctor’s schedule, which basically means you put your entire life on hold, never sure if a test date you need is going to pop up. Basically, you become afraid to plan much of anything in fear that your plans will interfere with your doctor’s schedule.
We’d already run the standard blood panels when we were hoping to save the ectopic pregnancy.
We learned I had a few blood clotting factors, which led my doctor to suggest taking baby aspirin, but the clotting factors were nothing that would’ve caused recurrent miscarriage.
So now my doctor settled on a new round of tests:
- Hysterosalpingogram (HSG) to check my fallopian tubes and uterus
- Karyotype testing to ensure both Husband and I carry normal chromosomal structures
- Endometrial Biopsy to check the health of my uterus
In Recurrent Miscarriage Madness, We Found Something!
Sweet baby Jesus, thank God almighty, WE FOUND SOMETHING!
This is how it feels when you’re going through recurrent miscarriage and you think you’ve found a cause.
Because only 50% of RPL patients ever find a cause for their losses, you’re desperate to finally be on the good side of the odds.
It’s not that you want to know something is wrong, except that . . . well . . . YOU DO!
Because knowing something is wrong means there’s something you can fix! And it might help! You might get a different outcome.
Through endometrial biopsy, we discovered chronic endometritis, a chronic infection in my uterus. What caused it? Who knows? I don’t even care. Just get rid of it, I thought.
So I took a serious regiment of stronger antibiotics than I’ve ever been on, and then we tried again, and I became pregnant.
We all knew this would be the time that I kept the baby safely in my uterus. We’d found the problem and fixed it. This would be the time.
Until it wasn’t. Until an ultrasound told us it wasn’t.
We were stunned. My doctor was stunned. As he delivered the news, his wife called. Since she was my doctor also, we told him to answer. He told her the news. We all wept.
How could it not have worked?
There was only one test left to do.
My doctor offered to administer methotrexate again because this one was SO small that it would still work, even though the pregnancy wasn’t ectopic. But before I had time to get back to the office, I had begun miscarrying naturally.
This was the 4th loss in our recurrent miscarriage journey.
Hysteroscopy: The Last Step In My Recurrent Miscarriage Workup
The only remaining test was a hysteroscopy. Some doctors have further immune protocols they’ll test for. But mine doesn’t practice Reproductive Immunology, so that would have been a whole new process to begin at a different clinic.
Thank God, the hysteroscopy is how we found what we believe to be the cause of my losses.
My Reproductive Endocrinologist, Dr, Shapiro, who I highly recommend to anyone in the Atlanta area, suggested this last step.
Most doctors wait to perform a hysteroscopy after all other tests have been exhausted because, in most cases, it requires full anesthesia, which comes with a number of risk factors.
I Got Lucky. Or, Fate Finally Finished Its Game
During my procedure, Dr. Shapiro noticed that my healthy-looking uterus was slightly arcuate. This essentially means that the top of my uterus was mildly heart-shaped, a normal variant that is not believed to cause pregnancy loss.
Knowing this wasn’t the cause of my problem, but also knowing this was the last procedure on our checklist, Dr. Shapiro decided to reshape my uterus.
He wanted to be able to tell me he’d done all he could.
Squeamish Alert: What’s coming might make your stomach churn, but it gave us Jack.
When he began reshaping my uterus, he made a surprising discovery: it didn’t bleed. So he continued snipping.
70% of my uterine wall was dead tissue that didn’t bleed when cut.
70%!!!!!
This means that any embryo that implanted in this 70% of my uterus would not be able to get proper blood flow to grow. And it was the area where embryos most often implant.
This. Was. Huge!
Dr. Shapiro snipped and snipped and snipped away at my uterine wall until my entire uterus bled. He then gave me pain medicine, said to rest, and wait 6 weeks to try again.
10 weeks later, I was pregnant with Jack.
A New Discovery?
Here’s the thing. Checking to ensure uterine wall bleeds is not on any recurrent miscarriage testing protocol list.
My uterus looked healthy. My doctor only did what he did because of my uterine shape and his desire to have done literally everything possible.
The discovery of this problem was chance. It was luck. Or it was fate.
I believe it was fate set in motion many years earlier when my OB had moved to California, and I had almost randomly selected his wife as my GYN. She was kind, empathetic, easy to see with a short wait at each appointment.
She connected me with her husband, who found a problem that doctors don’t know to look for! That he didn’t know to look for.
If I had a hysteroscopy on any other day, with any other doctor, or closer to lunch when he was hungry, or needed to get to his next embryo implantation, we never would’ve found this problem.
And we almost certainly wouldn’t have Jack.
Dr. Shapiro later told me that his clinic had begun lightly snipping a few different parts of the uterus as routine during hysteroscopy. Apparently, they’ve been shocked by how often they see this same problem.
How often? I don’t know.
How often did it solve the recurrent miscarriage problem? I don’t know.
Are they publishing research on it? I don’t know.
But I’m telling you because you need to know!
If you’re having a hysteroscopy to search for the cause of recurrent miscarriage, ask your doctor to do this!!!
It may not be the answer, but they’re already in there, and it only takes a few snips. Why NOT check?
Recurrent Miscarriage Support Resources
If you’ve read this far, chances are that you’re in the throws of RPL yourself. I am so, so, so sorry. Please reach out to me if you need me, have questions about my testing checklist, or just need to vent.
When I was experiencing RPL, I struggled so much to find helpful resources. That’s a huge part of what led me to launch Undefining Motherhood.
You shouldn’t have to experience the same problem, so I’ve listed a number of resources for you below. I want you to find what you need easily. God knows you deserve one less thing to worry about.
Chat with other members of the Undefining Motherhood community to find people who understand your experience.
We also have numerous other posts that are great resources for miscarrying mothers, their partners, and their support networks. Some of the top posts include:
- “What to Expect When Miscarrying”
- “How to Support Someone Through Miscarriage”
- “What (Not) to Say to Someone Who Had a Miscarriage”
If you think you’d benefit from mental health counseling, please reach out to Postpartum Support International for emotional support and help finding a therapist. Most postpartum mental health specialists are also trained in perinatal loss, so this is still the best resource, in my opinion.
Keep in mind that online support groups are made up mostly of women who haven’t found answers and are not medical professionals. Thus, be careful what advice you choose to take. Still, these people get you, and that’s huge. I cannot fathom having made it through my RPL experience without the support of women from the Facebook Group “Recurrent Miscarriage/Multiple Miscarriage Support.”
Love to you, mamas. And yes, you are mamas.

With our journal for the sisterhood of pregnancy loss, called Mourning Retreat, miscarrying mothers have the opportunity to work through their emotions and gain access to a private online community of women who have been in their shoes.











Thanks for writing this wonderful post. I am so thankful I found this because I am diagnosed with the same thing after 3 pregnancy losses and 2 Hysterscopys. I’m worried about the surgery. What is the recovery like? Your story gives me such hope
So interesting that you got the same diagnosis! Did they give you a name for it? Recovery was fine. I needed lots of pain meds when I woke up, then went home and took meds maybe for another day. Felt pretty normal after that.
So I’ve lost a 13week, (needed 2D&Cs) and a 9 week (1 D&C) and most recently an ectopic- would a D&C not do the same thing or no because it’s just scraping the inside? I’ve had a successful pregnancy 5 years ago and wondering if I bring this up to my reproductive endocrinologist if HES going to be like huh
I’m so sorry for your losses, Grace, and am here if you need an ear. Do you mean should you bring up why my hysteroscopy found? A D&C would not do the same thing. A D&C removes the contents of your uterus, while what I had done was an actual cutting away of the wall. That said, I would guess my problem is more likely with early losses. With later losses (2 D&Cs for one loss? Girl, you’ve been through the ringer!), I would be very more concerned about karyotype testing, blood clotting disorders, autoimmune disorders, and anatomical issues that can allow a pregnancy to progress (like a uterine septum.) The ectopic could be related to something like a septum or fibroid, or it could just be bad luck. (I hate it when people say that. I’m so sorry to say that, but cannot come up with better words.) All that you say, it sounds like it’s time for the full testing gamut, but I’d be surprised if our specific problems were the same. I should obviously caveat that I’m not a medical doctor, so these are my thoughts, but not medical advice. Also, seriously, you’ve been through Hell. Email me anytime if you need to talk.
Hi Katy! Thanks so much for sharing your story. I also have recurrent miscarriages (3 so far…one was a chemical, one i lost after hearing a heartbeat, and one was a blighted ovum). What did the doctor call your condition where the uterus had dead tissue? Did the doctor say how you developed this? I just have a gut feeling that when I do get pregnant, it’s not getting nutrients. I’ve gotten my miscarriage tissue tested and they never found a chromosome abnormality.
Hi Lacie! This is a great question, and I wish I had a better answer. Unfortunately, there was no name for my abnormality. My specialist said he’d never seen it before and never read about it in research, though they did start checking routinely during hysteroscopy and saw the same problem repeatedly. I hope there has been research on it since then, but need to follow up to find out. He simply explained it as not having any good red blood vessels in my uterine wall where embryos would attach, so they had to shave off the “dead” tissue until they got to tissue that bled. I know your doctor would much rather hear a medical term, but I like to hope that, by telling them the story, they’ll be willing to lightly snip a few places in your uterus during hysteroscopy to ensure bleeding. I hope this helps, and that I can come back with a better answer in the future as more research is done! I’m so sorry for what you’re going through. Reach out anytime you need someone to listen!
Hi Katy, I’m also 1 in a 100. 4 years, 5 pregnancies, 5 miscarriages- 8 weeks natural, 5 week chemical, 9 week D&C (Trisomy 15), 5 week chemical, and blighted ovum discovered at 8 weeks just two months ago in May 2020. In fact, your story felt so much like my own. Reading your story, I cried with you relating to all the emotions you wrote about feeling- I angry cried with your frustrations, I cried heartbroken for each one of your losses, and I cried in absolute rejoice to hear you were blessed with your perfect baby Jack. I just can’t express enough thanks for your bravery and strength to share this intimate journey with the world. It not only gives me hope but gives me direction and information to share with my providers attempting to find an answer of my own. (My doctor wants to do a hysteroscopy, hysterosalpingogram, and laparoscopy soon and I am going to bring up your case in our pre-op appointment next week.) I am so sorry for your struggles and your loss, I know that your child does not replace or negate the devastation you and your husband went through but I’m glad it gives you light and hope and happiness for your future.
Wishing you all the best,
Lindsay
Thank you so much for this sweet comment, Lindsay. I’m so sorry for all you’ve been through and hope your testing will provide the results you deserve and desire. Please keep me posted as you talk to your doctor or if you have any questions. Much love, Katy
I’m so sorry for your losses but so happy that you found an answer! My husband and I are trying for our 2nd child, our son turns 3 this month. I had a chemical before our son, healthy pregnancy and since we started trying again in fall of 2018 had a blighted ovum found at 9 weeks, a second chemical and now another blighted ovum. We are currently deciding on which direction to go with testing, but your story confirms my decision to have a D & C and test. If nothing else, it’s a starting point to move forward. Thanks for sharing your journey.
I’m so sorry you’re going through this but agree with your experience. Definitely check out our recurrent miscarriage testing article if you want guidance on that journey. https://undefiningmotherhood.com/recurrent-miscarriage-testing/
Hi Katy, thanks so much for sharing your story. I just wanted to let you know, as I also suffered from this condition, it’s called Asherman’s Syndrome or Intrauterine Adhesions, and it is an acquired condition most often caused by D&Cs or other uterine surgery, sometimes even by IUDs or infections. Essentially, the endometrium is scarred by whatever trauma (in my case the D&C), and the scar tissue grows on top of/instead of the regular endometrium. For some, like me, it causes your periods to stop altogether, as the scar tissue blocks the opening of the cervix and can also keep your uterine lining from building. It’s so frustrating, because D&Cs are always explained as such a low risk procedure. Since dealing with Asherman’s, and finding a specialist surgeon to treat it via hysteroscopy similar to what you experienced, I’ve learned it is much more common than people realize and yet the OBGYN field is extremely ill-informed on the condition. I’m so glad your RE was able to successfully remove the tissue. Many women have been further scarred by REs/OBs who do not know what they are doing. I really hope with your platform you can spread awareness on this condition and help others find answers and avoid the causes in the first place. Thank you!
Thank you so much for this helpful comment, and I’m so sorry for your experience. My RE said that my condition was not Asherman’s, and that it’s likely something I was born with, covering 70% of my uterus. None-the-less, your comment is so helpful because it is a condition very similar to Asherman’s, which highlights all the more why this is something our doctors need to check for. I hope many women will benefit from your story. Thank you for sharing!
Thank you so much for sharing your story, Katy. I am so happy my google search lead me here. With the exception of your ectopic I have unfortunately had almost the exact same experience. I had a saline sonohysteogram this week and was hoping to find something wrong but it came back with a arcuate uterus and I was told that wouldn’t be the issue. I felt devastated. I have not talked with my doctor yet but I am going to share your story with him and push to see if this is my issue. Again, thank you and congratulations on your healthy little Jack! 🙂
I am so sorry to hear of all the pain and trauma you have endured through your recurrent pregnancy losses. I’m so glad you finally got your baby, but I know that doesn’t erase the pain either.
I began reading your post because I have also had recurrent losses, but I was shocked when you said you see Dr. Shappiro! I see another doctor at the same office as Dr. Shappiro who also did a hysteroscopy on me. For me it was because we believed I either had a septum or scar tissue from a D&C. It turned out to be nothing more than an extremely small septum that the doctor said would not have caused the miscarriages. So far we have not found a cause (despite literal boatloads of bloodwork), but one of my losses was a complete molar pregnancy, so I obviously have genetic issues with some of my eggs.
It sounds like you have been through a lot. Recurrent pregnancy loss and all the testing and waiting that goes along with it are so draining emotionally. It can really wear you down. I am so blessed that I do have one living child, but I have had 3 losses since she was born (plus one before she was born). It is a heavy burden that we often bear alone, hiding and trying to protect ourselves. But I am learning through this process to trust God not for what I want Him to give me but for what He knows is ultimately best in a grand plan that I cannot possibly comprehend. I wrote about that in my most recent blog post: https://mamarissa.com/god-cares-about-your-miscarriage/
Thank you so much for being open and willing to share your experiences. As you mentioned, I never thought I would one day relate to a post like this. But here we are. And we are stronger for sharing with each other.